Personalized medicine: Emerging organoid models to better treat prostate cancer
Dr. Veronica Gil discusses how 3D cell culture is enabling scientists to develop and craft organ-specific tissues from stem cells to transform prostate cancer therapy
15 Apr 2021
In this exclusive interview, we learn about Dr. Veronica Gil’s work on the development and establishment of in vivo and 3D in vitro models to improve understanding of the mechanisms underlying advanced prostate cancer. Gil is a Higher Scientific Officer at the Institute of Cancer Research in London, where she works as part of the Cancer Biomarkers team led by Prof. Johann de Bono.
Developing organoids — to accelerate drug development, create novel cancer therapies, improve understanding of tumor biology, and examine drug sensitivity and resistance mechanisms — is challenging work. Gil reveals how her choice of pipettors has made that work more efficient and eased pains and strains associated with repetitive movements.
Modeling castration-resistant prostate cancer (CRPC)
Metastatic castration-resistant prostate cancer (CRPC) is an incurable and heterogeneous disease that makes up 10-20% of all prostate cancer cases. Depending on the grade of prostate cancer, disease progression can develop into castration-resistant cancer within 10 years. The median survival of CRPC ranges between 15 and 36 months. Medical advances have improved prostate cancer standards of care, which in turn has led to an increase in the incidence of CRPC. “It is key that we study new molecular-targeted and individually-tailored therapies to improve the treatment and the quality of life for patients,” Gil declares.
As tumors grow and evolve, cells can pick up new mutations, allowing them to evade immune surveillance or otherwise suppress the anti-tumor immune response. “Drugs that target checkpoints in the tumor microenvironment are potential new target approaches, for which patient selection is extremely important,” notes Gil. Yet CRPC models allowing researchers to study such things are scarce, and it is very difficult to grow models in vitro from primary tissues: “Significant challenges remain as we need to be able to generate individual growth conditions for each tumor.”
Gil and her team have spent years developing their own in-house xenograft models of tumors by implanting patient biopsies into NOD/SCID mice and gradually weaning them from androgens by sequentially passaging the tumors through other mice. It takes six to nine months to establish tumors that thrive in the absence of androgens.
A 3D route to targeted treatment
In addition to their use as in vivo models, the researchers can excise portions of the xenograft and plate them as single-cell suspensions. “By expanding these colonies, we can obtain fresh tumor tissue and grow the tumor as organoids in vitro for our studies. For this purpose, we widely use Corning Matrigel and the hanging drop techniques,” Gil explains. “We isolate single cells from these tumors, seed them into Matrigel, generate the hanging drop, and the organoids will form within five to ten days.”
3D cell cultures, sometimes known as spheroids or organoids, offer advantages over planar cell cultures at activating mechanotransduction and proliferative pathways exhibited by in situ tumors. “It is the best model so far to resemble the tumor growing in the patient,” says Gil. Such models enable her to explore a potential drug’s efficacy by targeting checkpoint proteins involved in anti-tumor immunity, as well as by dissecting the addiction of advanced tumors to specific pathways that promote progression and treatment resistance.
Gil is hugely positive about potential advances that could soon materialize in the field of precision medicine. “I think that by means of this fast-advancing technology in disease modeling, and by working closely together with key collaborators around the world, I hope we could develop the perfect tumor model in vitro to match each individual patient's targeted therapies, for them to have the best possible chance of success in disease treatment and to follow patients from bench to bedside.”
Changing working life for the better
The road ahead requires the comparison of multiple replicates of several cultures under various conditions at different time points. “The organoid work – 3D biology – is very precise and it’s a lot more complex than the traditional 2D culture,” Gil explains. “So, you spend many hours with this precise pipetting, and seeding and treating organoids. It can be exhausting for the body. Gil reveals how her choice of pipettors has made that work more efficient and eased pains and strains associated with repetitive movements.
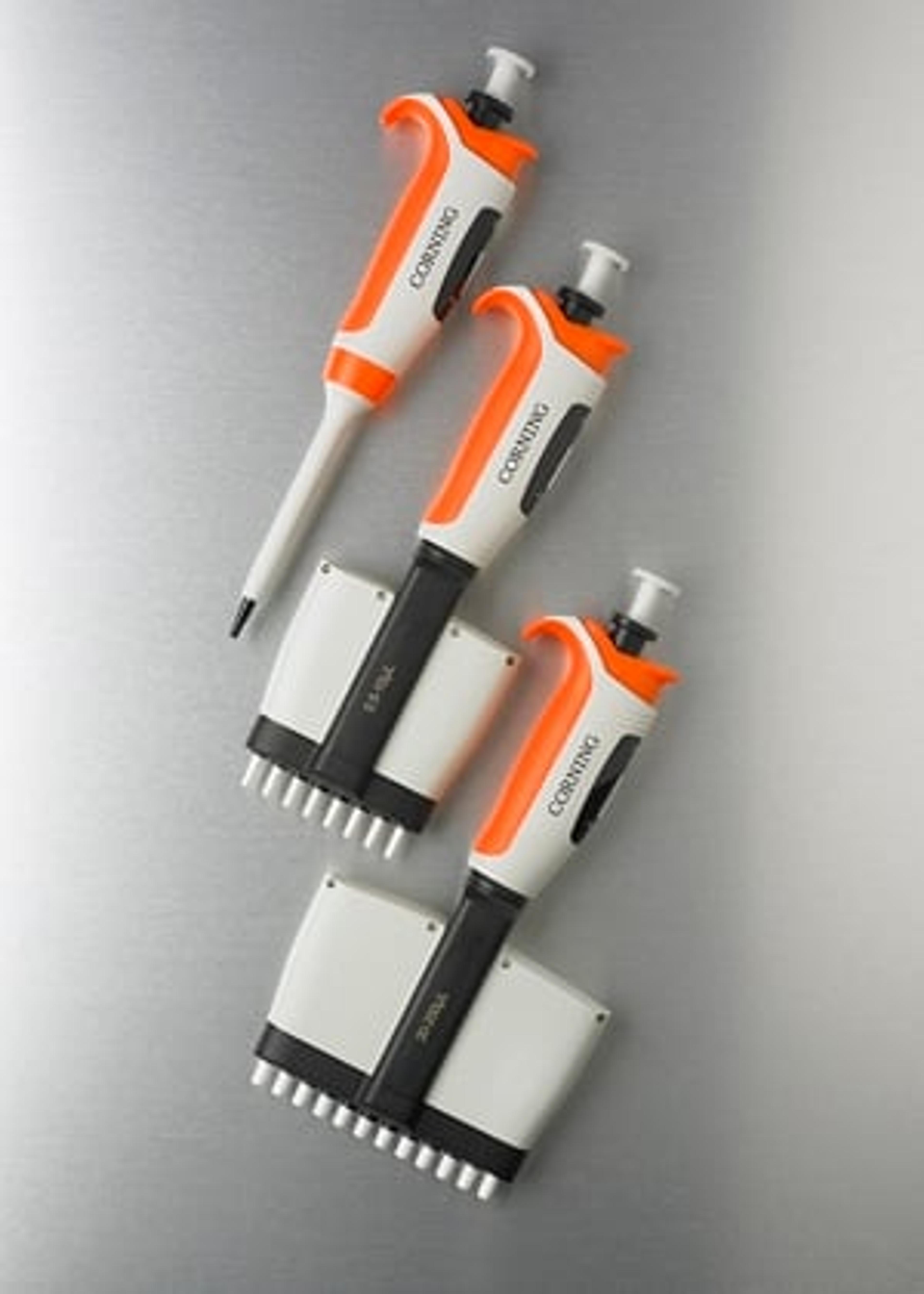
Gil discovered Corning Lambda Elite Touch pipettors about a year ago. “I’m glad I found them,” she says. “These pipettors have improved my working life. I have chronic postural neck pain due to so many hours working in the hood and their ergonomic properties, the ease of use, made a big change for me. They are lightweight. The low force needed to operate the pipette has certainly helped avoid neck, arm, and wrist muscle strains. They’re really good.” These more ergonomic pipettors also help Gil with productivity. Setting up an organoid slab takes a while. “Almost like an artisan,” you have to very slowly maximize the even seeding of these organoids because they are all heterogeneous in size and number. These pipettors don’t quite make the task high throughput, “but you can manually do more in a shorter period of time,” explains Gil.
Ultimately, if all the work pays off, it will be fantastic to “have the tumor of the patient growing in vitro as a mini-tumor in the lab,” and to then treat the patient based on your pre-clinical in vitro study. Then you are a step ahead, says Gil — that is truly individualized treatment.
References
- New Non-Metastatic, Castration-Resistant Prostate Cancer Treatment. Oncology Time. March 2018
- He, Lugeng MD; Fang, Hui Ph.D.; Chen, Chao Ph.D.; Wu, Yanqi Ph; Wang, Yuyong Ph.D.; Ge, Hongwei Ph.D.; Wang, Lili Ph.D.; Wan, Yuehu; He, Huadong Ph.D., Metastatic castration-resistant prostate cancer. Academic insights and perspectives through bibliometric analysis, Medicine. April 2020
- Crawford, E.D.; Petrylak, D.; Sartor, O. Navigating the evolving therapeutic landscape in advanced prostate cancer. Urol. Oncol. 2017
- Kirby, M.; Hirst, C.; Crawford, E.D. Characterising the castration-resistant prostate cancer population: A systematic review. Int. J. Clin. Pract. 2011