Neurological Regenerative Medicine – Unlocking the Potential of Stem Cells in the Olfactory System
Learn how stem cell biologist Dr. Barbara Murdoch’s research into our sense of smell could help develop new neurodegenerative disease therapies
24 Apr 2017
Source: www.123rf.com

Barbara Murdoch, Ph.D. Dr. Murdoch is a stem cell biologist with an interest in development and regenerative medicine. After completing post-doctoral training at Yale University, she took the role of Assistant Professor at Eastern Connecticut State University, where her time is split between teaching and researching nervous system development.
As our understanding of stem cells has increased, the possibility of using stem cell therapies to treat disease is on the horizon. Barbara Murdoch, Ph.D., Assistant Professor at Eastern Connecticut State University, is studying stem cells found in the olfactory epithelium (OE) with the aim of finding therapies for neurodegeneration.
Exclusive neurogenic niche: The olfactory epithelium
The OE is one of the few tissues in the body which is known to regenerate neurons, preserving our sense of smell throughout our lives.
“Have you ever had the experience where you smell something and the scent evokes a memory from years back in time?” asked Dr. Murdoch. “This is because not only can the stem cells in the OE divide and differentiate to replace the lost neurons, but they can also recreate the exact same connection in the brain as the neuron they are replacing.”
Dr. Murdoch explained how by studying these stem cells, she hoped to elucidate the environment and signaling molecules which restrict them to certain cell fates. The aim of her research is to direct neural stem/progenitor cells to create neurons in vitro. “We can transplant neuronal precursor cells which are on their way to make neurons into patients, for example to help them recover after a stroke,” said Dr. Murdoch.
Development of the olfactory epithelium approaches
One approach to understanding what dictates cell fate is to investigate the regions enriched for progenitors and determine their local microenvironment. The communication signals forming the microenvironment can be used to drive the production of new neurons from neuronal precursors in vitro. To investigate olfactory development, Dr. Murdoch carries out confocal microscopy using antibodies against numerous cell markers such as nestin, β3-tubulin and GFAP.
“I was at a meeting when, just by chance, I came across a representative from Covance (now BioLegend) who had an anti-nestin antibody and was kind enough to give me a sample. When I tried it, it was brilliant in the olfactory epithelium and the brain,” said Dr. Murdoch.
The stem cells in the olfactory epithelium can recreate the exact same connection in the brain as the neuron they are replacing.
Dr. Murdoch published her findings in the 2008 Journal of Neuroscience paper, demonstrating that there were stem cell-like cells in the embryonic OE which are very similar to neural cells in the brain known as radial glia cells. Radial glia are responsible for the production of most if not all neurons in the brain. Previously, it was thought that radial glia cells were restricted to the central nervous system, but Dr. Murdoch’s research shows that they are also present in the OE, which is part of the peripheral nervous system.
“The reason I think this was missed by so many other researchers was that the antibody that was typically used as a marker of neural stem cells, the anti-nestin antibody, worked well in the brain but not very well in the OE,” Dr. Murdoch explained. However, the new antibody from BioLegend was targeting a different epitope, allowing it to identify and bind well to nestin expressed in the OE.
Dr. Murdoch described finding effective primary antibodies as a somewhat ‘hit or miss’ process. “Often when I’m searching for antibodies, I try to get a sample and test it with the organism and tissue type I’m using. When you find antibodies that work, you stick with them. That’s the reason why I stick with the antibodies from BioLegend, as they are so specific time and time again,” Dr. Murdoch added.
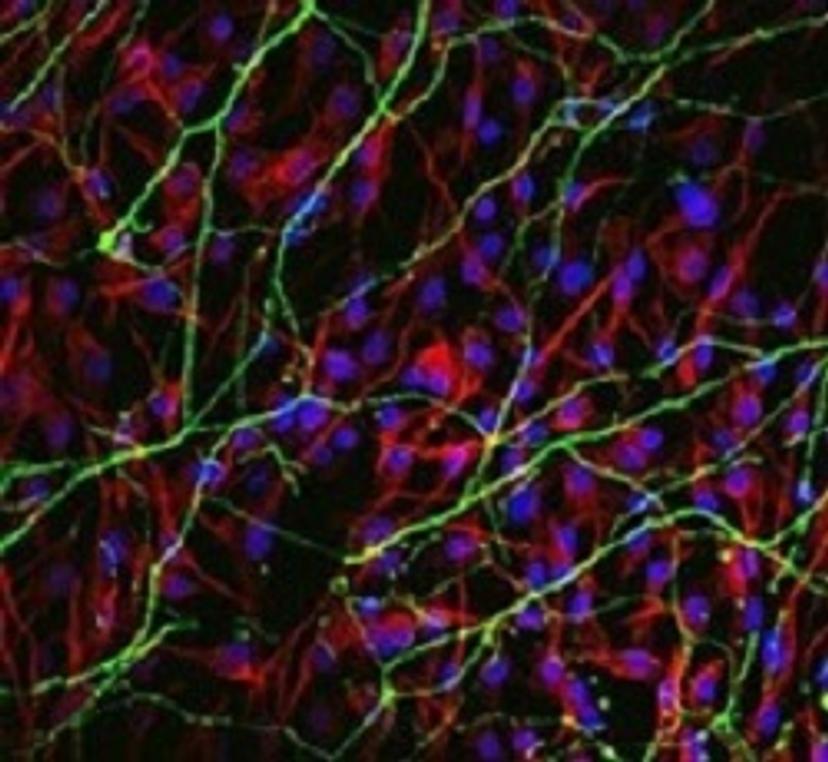
Confocal image of chicken embryonic neural progenitors grown in vitro The image shows differentiation into neurons (green) and glia (red). Blue indicates cell nuclei. Provided by Dr. Murdoch.
Future research and application in regenerative medicine approaches
Now an Assistant Professor at Eastern Connecticut State University, Dr. Murdoch is furthering her research by using chick embryos as a model to study how the OE develops.
“We’re trying to find pockets of progenitor cells and learn what the environmental influences surrounding those cells are in vivo,” Dr. Murdoch explained.
“This research has implications for regenerative medicine, where the same signals found in vivo can be recreated in vitro to make new neurons from neural precursors, derived either from human embryonic or induced pluripotent stem cells. Future work will aim to construct 3D scaffolds combined with signaling molecules and matrices to affect cell fate,” Dr. Murdoch said.
Research such as Dr. Murdoch’s is contributing to an improved understanding of the signaling cascades found in neurogenic niches. Understanding the factors which decide cell fate and coordinate the generation of complex tissue is an important step in developing stem cell therapies to treat neurodegenerative states, such as Parkinson’s disease, traumatic brain injury and stroke.
Dr. Murdoch’s work is funded by the CSU-AAUP.
