Disrupting protein-protein interactions to rewrite transcription
In this guest editorial, Dr. Katherine Bridge, University of York, explains how aptamers could unlock new opportunities for more targeted and effective cancer treatments
20 Oct 2025
Dr. Katherine Bridge is a Kay Kendall Leukaemia Fund Intermediate Research Fellow at the University of York
Dr. Katherine Bridge is a Kay Kendall Leukaemia Fund Intermediate Research Fellow at the University of York. She is using binders developed by Aptamer Group to investigate the role of the Hypoxia-Inducible Factors (HIFs) transcription factors in blood cancer, with the potential to improve cancer treatment with targeted therapeutics. We spoke with her to find out how she sees aptamers as having a unique potential to improve cancer treatment.
What is the key research focus of your fellowship?
I am a Cancer Cell Biologist studying the role of HIFs in blood stem cells and blood cancers. One of the core things that we’re looking at in my lab is the context-dependent function of HIF transcription factors.
In cancer, HIF can be very oncogenic, driving cell proliferation and making the cancer more aggressive. However, there are some less common but well-documented cases where HIF functions to suppress the tumor instead. In these states, inhibition of HIF either pharmacologically or via knock-out results in acceleration of the tumor’s growth and aggressiveness.
My group is actively working to further understand how this one transcription factor can have such polar opposite roles in different contexts. We want to uncover the biology that explains how HIF is able to act as both a tumor oncogenic and suppressive factor. These research findings could present a key opportunity to therapeutically target HIF as a transcription factor, with the potential to switch it from oncogenic HIF into tumor-suppressive HIF.
How did your interest develop in this research area?
As a post-doctoral researcher at the Cancer Research UK Barts Centre in London, I worked on the molecular mechanisms regulating HIF in lung cancers. Despite the power of this model system to characterize oncogenic HIF function in these tumors, it could not explain how and why HIF activation in other contexts (e.g., clear cell renal cell carcinoma) was tumor suppressive.
This prompted my move to the hematopoietic (blood) system, where we can use stem cells (both healthy and cancerous) in robustly established single-cell assays to analyze defined fate choice outcomes. Collaborating with Professor Ian Hitchcock and Dr. David Kent, established experts in the field of haematological malignancies here at the University of York, facilitated my transition from solid cancers to blood cancers, and created a new opportunity in which to address these fundamental biological questions.
Have you found it difficult building a career as a female in the male-dominated field of life sciences?
At the early stages of life science research, during my undergraduate and PhD research, I found there to be approximately equal numbers of men and women in the life sciences; however, as I’ve progressed, I have found that I have fewer female peers. For me, the environment is key: having colleagues who are actively promoting me and are keen to collaborate is essential. I didn’t really have female mentors as a junior researcher, and this is something I have now actively sought for myself. I am also passionate about mentoring the next generation of female scientists and facilitating access to biomedical research for underrepresented groups.
How were you introduced to aptamers as research tools?
One of my colleagues at the University of York, Dr. Michael Plevin, introduced me to aptamers. His lab is focused on the biology of protein-protein interactions, particularly in microRNA biogenesis, and I have worked on the microRNA pathway previously from a cellular perspective.
Michael and I started a collaboration with Aptamer Group to generate an aptamer to a specific subunit of DICER. Michael’s group is currently investigating the protein chemistry.
This research has been difficult over the past couple of years with the COVID pandemic, multiple lockdowns, and the slow returns to the lab. But for me, this exposure to aptamers sparked an interest in the potential application of aptamers to disrupt protein-protein interactions. To my knowledge, this hasn’t been extensively explored, but it could offer key insights into my lab’s research on the context-driven roles of HIF.
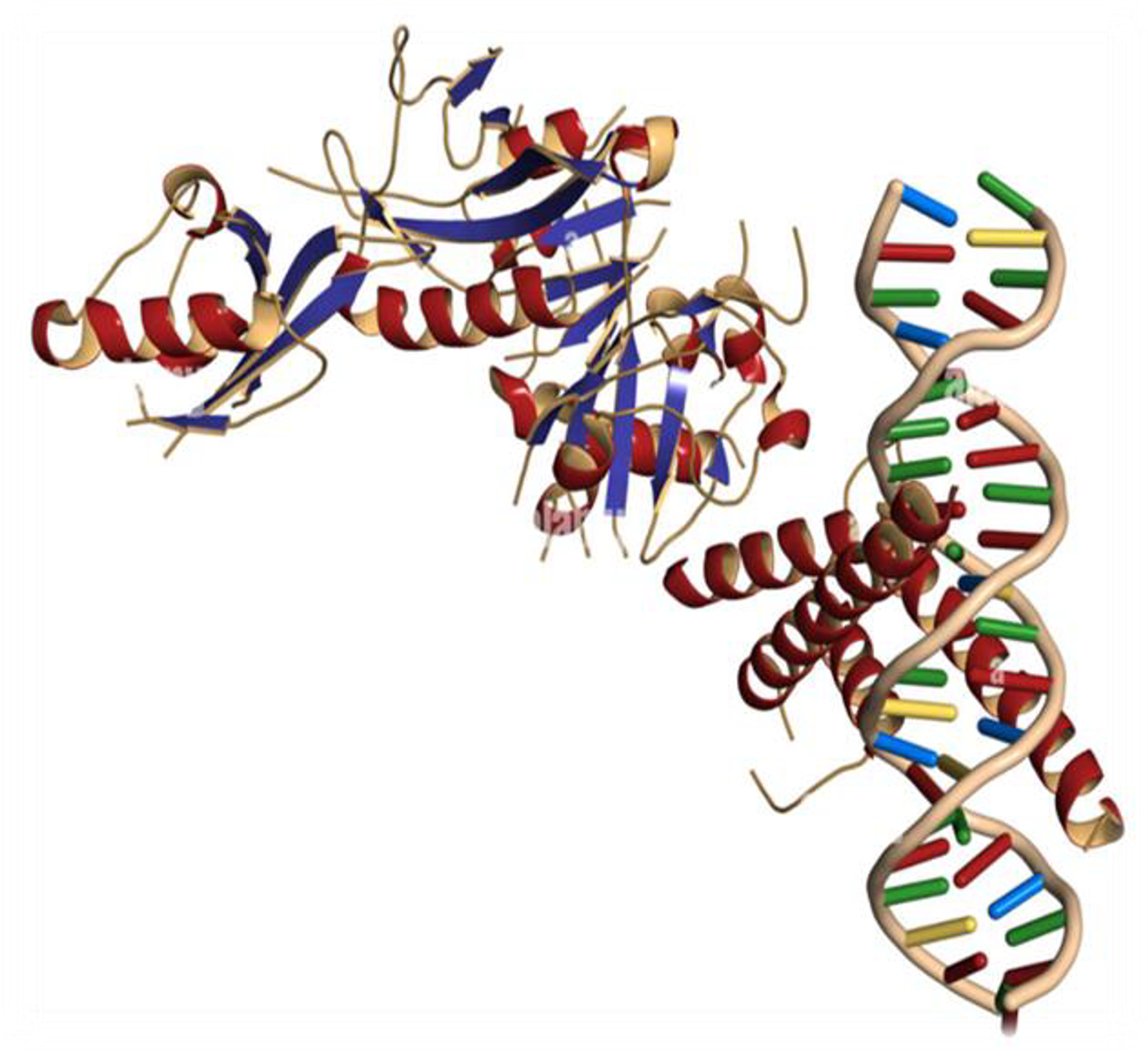
Aptamers to the transcription factor HIF-1α could offer new therapeutic modalities to treat disease such as cancer that stem from this previously undruggable target class.
How do you intend to use HIF-targeted aptamers in your research?
We are applying the target-specific aptamers to explore the function of HIF in a way that a drug or an antibody could not; potentially allowing us to direct its transcriptional function. This project serves as a proof of principle for a larger therapeutic question with regard to being able to target transcription factors. Even as close as five years ago, people said that transcription factors were not druggable. Nonetheless, given that transcription factors act as cellular drivers of phenotype and function, the potential to be able to modulate this behavior in a disease setting is very attractive. I think an aptamer could carry out this function in a way that a drug or an antibody could not. Aptamers to the transcription factor HIF-1α could offer new therapeutic modalities to treat disease such as cancer that stem from this previously undruggable target class.
How do you see aptamers as different to alternative therapeutic formats, such as small molecule drugs or large molecule antibodies?
In the context of therapy, the main differences between aptamers and antibodies or small-molecule therapeutics are side effects and toxicity. As aptamers are oligonucleotide-based molecules, they lack the toxicity and/or off-target effects of a small drug. The degree of specificity that you can achieve with an aptamer is uncommon to find in small-molecule drugs.
Antibodies are good at targeting cell surface proteins; they are used in this way as cell markers, and we’re beginning to see their function for targeted drug delivery to a particular type of cell, based on cell receptor recognition. But what antibodies fail to do, just because of the nature of their size and chemistry, is penetrate the cell interior to modulate the function of signalling pathways and phenotypes.
Is working with aptamers different than working with antibodies?
Aptamers and antibodies are quite different, and it’s important to remember that when we work with these tools. Like most researchers in the life sciences, I have worked with antibodies for years, but aptamers offer an alternative solution. Aptamers bring a smaller size to penetrate tissues further, the potential to hit new targets that antibodies can’t be developed to, and functionality to track endogenously in cells and organisms, like we are doing.
The team at Aptamer Group has been hugely supportive in developing these methods and sharing tips and techniques, but we are at the cutting edge of research, so many of these techniques and targets are very new.
What motivated you to work in this field?
I have worked on the HIF transcription factors and their role in tumorigenesis since my PhD studies and throughout my post-doctoral research, so their functions are critical questions for me. Having a basis in that scientific field, I naturally wanted to extend that research during my fellowship. Coming to York offered me a unique combination of cellular and molecular tools to underpin the development of a novel system for studying HIF as part of my Kay Kendall Intermediate Fellowship in the York Biomedical Research Institute.
A more personal motivation involves the recent passing of a family member from leukaemia. Watching them endure the chemotherapy treatment that was the only option motivated me to work towards better therapeutics. The reality of most cancer treatment remains chemotherapy, which utilizes drugs that target fast-growing cells and cause huge collateral damage to the rest of the body. Seeing how unwell they were at the end, not because of the cancer, but because of the treatment, made me want to explore new options and create new solutions. Aptamers could hold the potential for this.
